The extreme price of prescription drugs in America
Comparing over-the-counter prices of drugs in the U.S. and France

Living in France I still regularly hear stories about Americans’ experiences with healthcare—often focusing on the extraordinary cost of prescription drugs. The most recent tale involved a prescription for a three-month supply of Eliquis (Apixaban) for a person using a Medicare Advantage plan. The insurer had provided a “Copay card” pre-loaded with $750 to be used when purchasing drugs. The Eliquis prescription turned out to cost $1,781—so paying for the prescription required $1,031 out of pocket.
I then looked up the comparable over-the-counter cost for Eliquis at pharmacies in France, for the same dosage: it was €176.85, or about 10 percent of the cost in the United States. In fact, if we were prescribed Eliquis by a doctor here in France, our cost at the pharmacy would be zero, thanks to the single-payer health insurance system and our low-cost supplementary insurance (generally referred to as a mutuelle).
How could there be such an extraordinary difference?
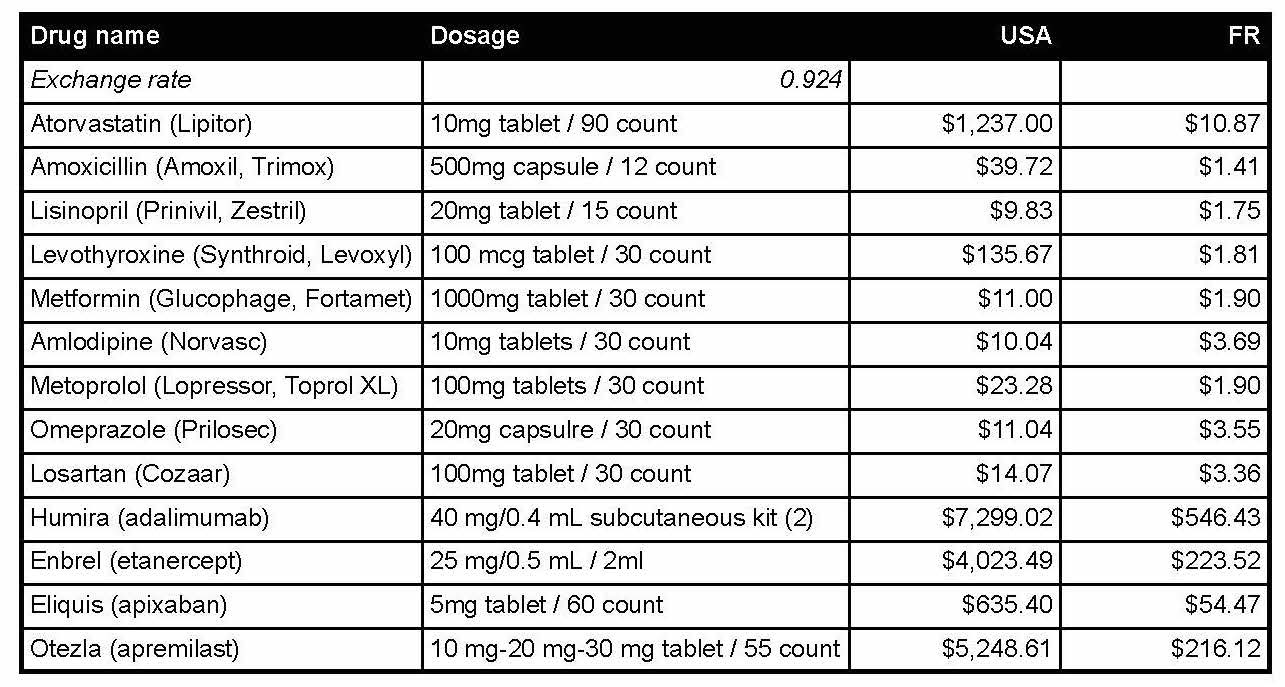
I’ve since compared the costs of fifteen prescription drugs in the U.S. and in France according to two reliable purveyors of drug information. Ten of the drugs are among the most commonly prescribed by American doctors; the others were chosen arbitrarily, but are also frequently prescribed, often for more specialised conditions. The results are shown in the table below.1
The result, in aggregate, is even more astonishing than the initial comparison made with Eliquis—on average, the cost of the very same drugs (brand and dosage) in France was less than 6 percent the cost in the United States.
There is something wildly wrong here. Let’s consider some reasons why.
First and foremost, France has a single-payer health insurance system—the Assurance Maladie, or more formally Caisse Primaire d’Assurance Maladie (generally referred to as CPAM). This means that there is a single public-sector entity nationally that is authorised and positioned to negotiate drug prices for the whole of French society—and obviously it does so effectively.
Second, there is genuine competition among the private insurers that provide supplementary health insurance. These organisations, consisting mostly of non-profits and private for-profit insurance companies, provide policies that cover costs that are not fully covered by CPAM. These organisations number in the hundreds. The high level of competition means costs are generally low, and consumers can evaluate many offerings to find one that fits their specific needs. If an individual or family cannot afford supplementary insurance, policies for those in need are also available from a range of public- and private-sector organisations.
The Biden administration and the Democratic Party have trumpeted advances made in the past several years in lowering costs of prescription drugs for Medicare subscribers. Specifically this includes authorising Medicare—the country’s existing single-payer medical insurance system—to negotiate prices with drug companies. It also includes lowering the cost of insulin for those over age 65 to $35 monthly, and capping overall annual expenditure on prescription drugs (with some exclusions) to $2,000.
But let’s put this into perspective. Medicare represents less than 20 percent of the U.S. population, so impact is limited. Many with Type 1 diabetes are diagnosed with the illness as adolescents, and the average age for diagnosis of all types of diabetes is 49.2 This means that some parts of the population are denied beneficial costs for insulin reserved for seniors for 15-50 years while suffering from both the disease and the costs of treatment. As a result, some will perish before qualifying for Medicare, and many others will suffer financial hardship. Also consider that many Americans over the age of 65 and living in retirement depend exclusively for income on Social Security. The average individual Social Security payment as of January 2025 is $1,976 (before taxes).3 So, the cap on drug payments of $2,000 annually will, for many, consume an entire month’s pre-tax income, or more.4
So the government’s efforts to lower drug prices in the past four years on behalf of its over-65 population have been extremely modest. Why? It is because the government and its leadership, regardless of party, also serve another powerful constituency—the private insurers who dominate the Medicare Part D marketplace, and who also control the industry that performs medical coding, prescription benefits management and the direct issuance of drugs to clients by their pharmacies. Indeed, a Federal Trade Commission report released 14 January 2025 concludes that pharmacy benefit managers (PBMs) were responsible for eye-watering increases in the cost of drugs for treatment of cancer, heart disease, HIV, and other illnesses. The report
found that the ‘Big 3 PBMs’—Caremark Rx, LLC (CVS), Express Scripts, Inc. (ESI), and OptumRx, Inc. (OptumRx)—marked up numerous specialty generic drugs dispensed at their affiliated pharmacies by thousands of percent, and many others by hundreds of percent. Such significant markups allowed the Big 3 PBMs and their affiliated specialty pharmacies to generate more than $7.3 billion in revenue from dispensing drugs in excess of the drugs’ estimated acquisition costs from 2017-2022. The Big 3 PBMs netted such significant revenues all while patient, employer, and other health care plan sponsor payments for drugs steadily increased annually, according to the staff report.5
(The report details other abuses as well as the cost impact on plan sponsors and individual plan participants.)
These companies and their shareholders, as well as their strategies to influence members of government, actively combat meaningful change in the American prescription drug market. They also promote sales of prescription drugs through unrelenting advertising (illegal in the European Union) and similarly encourage physicians to prescribe their products with gifts of swag and free samples of medications.
There is an argument that the best way forward for citizens of the U.S. is a transition to a comprehensive public-sector single-payer health insurance system, often referred to as “Medicare for All.” However, the current Medicare model falls short because its authorisation to negotiate drug prices with manufacturers is limited and because the drug payment benefits of Medicare Part D has been largely given over to the private sector which, arguably, acts on behalf of shareholders primarily and for its customers secondarily. So it is not the optimal model to replicate in comprehensive a single-payer system.
The solution is not just a transition to a comprehensive single-payer system. A thorough regulatory review that addresses the full range of abuses now rampant throughout the health insurance industry and among healthcare providers is badly needed. Unless these more holistic reforms are undertaken, a single-payer system could potentially perpetuate many of the economic and healthcare abuses that currently exist. Transitioning to a public-sector single-payer system is not as trivial a transition as some maintain. This is because, for many corporations and entrepreneurs, the very notion of the government operating a social welfare system of any kind flies in the face of their concept of “free enterprise” and a lightly regulated marketplace. Resistance from private-sector industrial stakeholders will be fierce.
It doesn’t have to be this way.
Unfortunately, what’s still missing is genuinely overwhelming public support for reform and the political will to get it done.
For consistency, costs were captured from the websites of two services providing comprehensive drug databases and therapeutic information to medical professionals and consumers alike. For France, I consulted the website of Vidal Group, https://www.vidal.fr/ and for the U.S. I consulted Drugs.com, which identifies itself as “the largest, most widely visited, independent medicine information website available on the Internet.” https://www.drugs.com/. Costs given in Euros were converted to U.S. dollars using the IRS avergae conversion rate for 2024 of €1 == $0.924. (consulted 18 Jan 2025)
Wang MC, Shah NS, Carnethon MR, O’Brien MJ, Khan SS. “Age at Diagnosis of Diabetes by Race and Ethnicity in the United States From 2011 to 2018.” JAMA Intern Med. 2021;181(11):1537–1539. https://doi.org/10.1001/jamainternmed.2021.4945 (consulted 18 Jan 2025)
“What is the average monthly benefit for a retired worker?” Social Security: Frequently Asked Questions (2 January 2025) https://www.ssa.gov/faqs/en/questions/KA-01903.html (consulted 18 Jan 2025)
Many households depend exclusively on Social Security for income after age 65. A study by Irena Dushi, Howard M. Iams, and Brad Trenkamp, “The Importance of Social Security Benefits to the Income of the Aged Population,” observe that in the 2015 Current Population Survey “about one-quarter of the aged population lived in families that received 90 percent or more of their family income from Social Security benefits.” Social Security Bulletin, Vol. 77 No. 2, 2017 (released May 2017) https://www.ssa.gov/policy/docs/ssb/v77n2/v77n2p1.html (consulted 18 Jan 2025)
Federal Trade Commission, “FTC Releases Second Interim Staff Report on Prescription Drug Middlemen: Report finds PBMs charge significant markups for cancer, HIV, and other critical specialty generic drugs,” FTC Press Releases (14 Jan 2025) https://www.ftc.gov/news-events/news/press-releases/2025/01/ftc-releases-second-interim-staff-report-prescription-drug-middlemen. See also Steve Kopack and Adiel Kaplan, “Top three insurers reaped $7.3 billion through their drug middlemen's markups, FTC says,” NBC News: Health News (14 Jan 2025) https://www.nbcnews.com/health/health-news/top-three-insurers-reaped-73-billion-drug-middlemens-markups-ftc-says-rcna187640 (consulted 18 Jan 2025)




Excellent post. Americans are fools. We are exceptionally good at shooting ourselves in the foot. Maybe by the time we are as old as Europe - when we grow up - we'll "get it".
This article helped me better understand something I always find shocking, but have trouble getting my head around. Thank you!